Inflammatory bowel diseases, also known as IBD, represent a group of autoimmune diseases that lead to chronic inflammation in the gastrointestinal (GI) tract. The two main diseases associated with this group are Crohn’s Disease and Ulcerative Colitis. Chronic inflammation ultimately damages the GI tract, resulting in symptoms that are often painful.
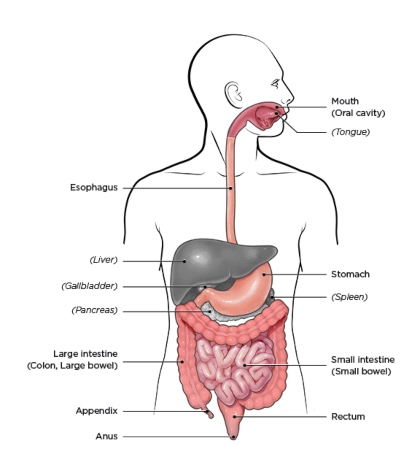
IBD can affect any portion of the GI tract.
Differences Between these Two Diseases
Although the symptoms are similar, several differences exist between these two diseases. A gastroenterologist must diagnose both conditions to avoid misdiagnosis. Crohn’s disease can occur anywhere along the GI tract, from the mouth to the anus. Typically, the most common area affected is the small intestine, just before the colon (ileum).
Inflammatory Bowel Diseases Affected areas present patches of irritation next to healthy tissue, and inflammation may penetrate through multiple wall layers within the intestine.
In contrast, Ulcerative Colitis is localized to the colon and rectum. Unlike the patchy areas seen in Crohn’s, the damaged regions in Colitis appear in a continuous pattern, typically moving upward from the rectum to the colon. Furthermore, Colitis only impacts the innermost wall of the colon, rather than affecting multiple layers.
Like most autoimmune diseases, researchers do not fully understand the cause(s) of IBD. Environmental and genetic factors likely contribute to the condition. This combination triggers an immune response that attacks the cells in the GI tract. Moreover, the symptoms of IBD are similar in both Crohn’s and Colitis, which can often lead to misdiagnosis.
Common Symptoms:
• Persistent diarrhea
• Abdominal pain
• Rectal bleeding/bloody stools
• Weight loss
• Fatigue
IBD is different from, Irritable Bowel Syndrome and Celiac disease.
IBD is distinct from Irritable Bowel Syndrome and Celiac disease. Similarity in the symptoms can lead to misdiagnosis, which is why seeking a physician for an accurate diagnosis and appropriate treatment is essential. Now that we understand how IBD can affect us, let’s explore its potential impact on oral health. IBD can manifest in several oral conditions:
Xerostomia (Dry Mouth): The salivary glands may not produce enough saliva to keep the mouth moist and maintain the pH balance of the oral cavity. This condition can result in rampant decay.
Aphthous Ulcers: Also known as canker sores, individuals with IBD may experience frequent or multiple ulcers. These lesions can make oral care uncomfortable.
Mucosal Tags: Similar to skin tags, these can develop as a result of Crohn’s Disease. They may appear on the inner cheek and can be visualized by your dentist or hygienist.
Gingivitis: This reversible form of periodontal disease can be treated with good home care and regular professional hygiene visits.

Best Suits Your Dental Needs.
Depending on which manifestations you’re experiencing, your doctor and hygienist will tailor a treatment plan that best meets your dental needs. For example, if you frequently develop aphthous ulcers, they may prescribe a steroid cream to reduce their duration and frequency.
If you suffer from xerostomia, we will discuss the best options to balance your pH and decrease your risk of decay. Similarly, if you have an autoimmune disease, maintaining good oral health will help reduce its impact on your immune response.
Furthermore, if you would like to discuss how your IBD may be affecting your oral health, please feel free to mention it at your next visit.
References
Faster, better, and more comfortable care is available at Dental Care Of Sumner. We truly live up to our name with an office packed full of advanced technology and a team who is helping move dentistry into the 21st century.